The pandemic has highlighted our nation’s continuing struggle with health equity.
According to the CDC, the number of individuals who have died from COVID-19 in the U.S. are disproportionately “Hispanic or Latino, non-Hispanic Black, and non-Hispanic American Indian or Alaska Native.”1 These underserved minority groups are victims of ineffective policies and a failed healthcare delivery system, the impact from which includes reduced access to affordable care, increased chronic disease, and poorer outcomes. 2
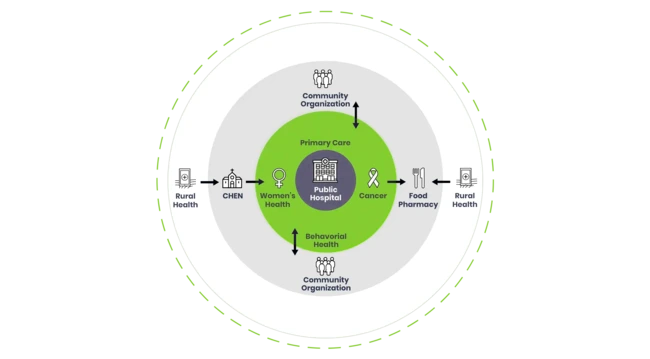
The good news is that progress is being made—just not where some might suspect. Instead of large health systems with well-funded foundations, the most innovative transformations have come from public safety net hospitals— so called “last resort” hospitals. At a time when others talk about using innovation to reduce health inequity, address disparities, improve the health of populations, and reduce costs; community hospitals have succeeded in building a highly effective model. What they’re doing is quite remarkable and completely repeatable in communities across the country.